

PROVIDER CREDENTIALING
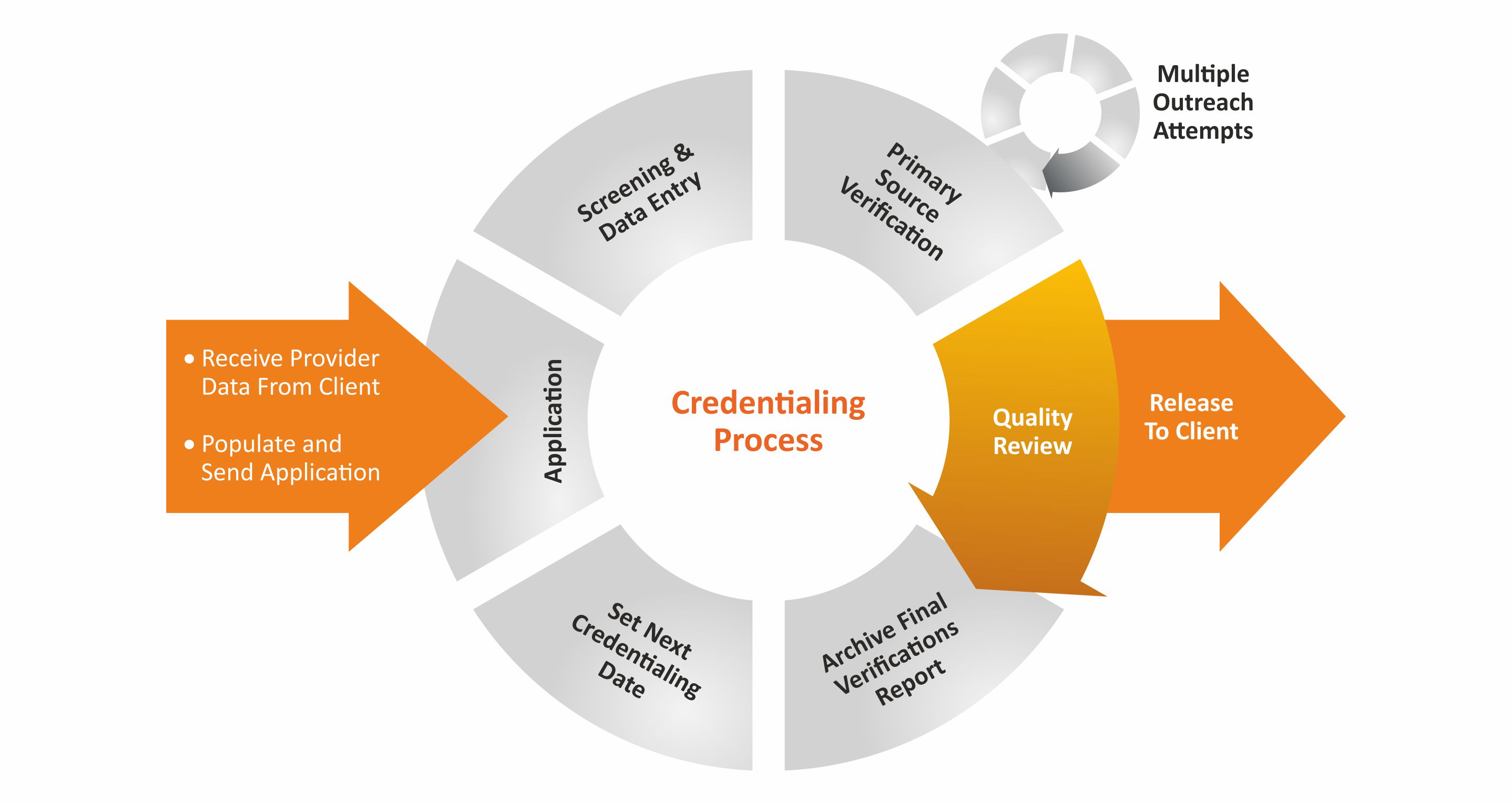
Enrollment and credentialing are critical parts to a successful medical billing operation. Missed deadlines and incorrect documentation can make this time-consuming process a nightmare. This is a very critical function for the providers to become a part of a payor network and to receive better revenue realization. Our experienced staff thoroughly and meticulously performs the credentialing for providers by reviewing the necessary documents and filling out the required forms.

ELIGIBILITY & BENEFITS
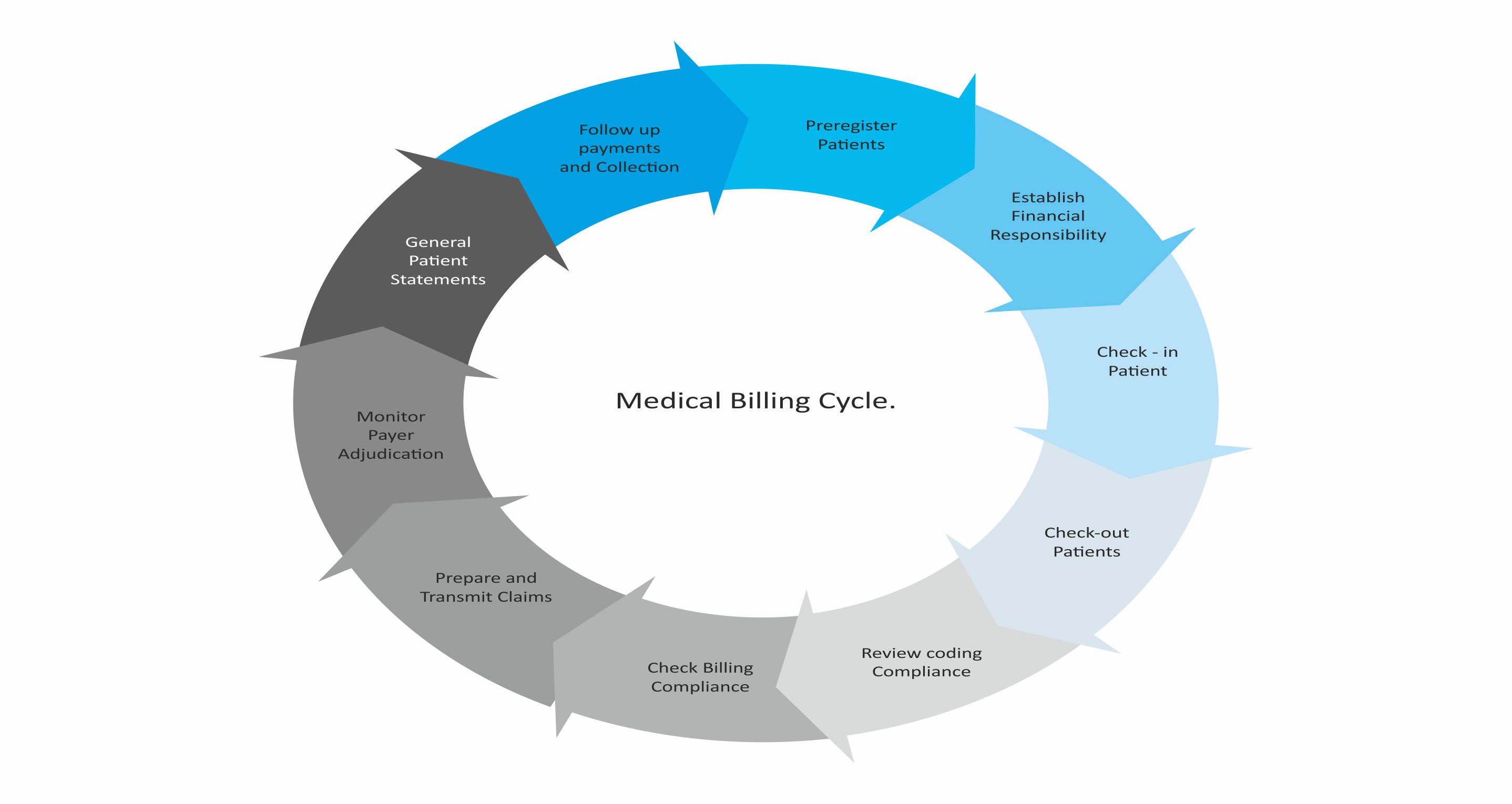
Front office before pre visit collects insurance information. And this is fed in EMR and it is cross checked with insurance to confirm Active or inactive Insurance status. So front desk can inform Patient for collecting copay and patient responsibility. Initiating a solid insurance verification process in place can reduce the denials and makes medical billing process more efficient.
Physicians need to verify each patient’s eligibility and benefits to ensure they will receive payment for services rendered.In the era of high patient deductibles, we help take on the heavy lifting of gathering both eligibility and benefits before the patient visit. This is an essential service for your clients as they struggle with increasing patient payment responsibilities.

PATIENT DEMOGRAPHICS ENTRY
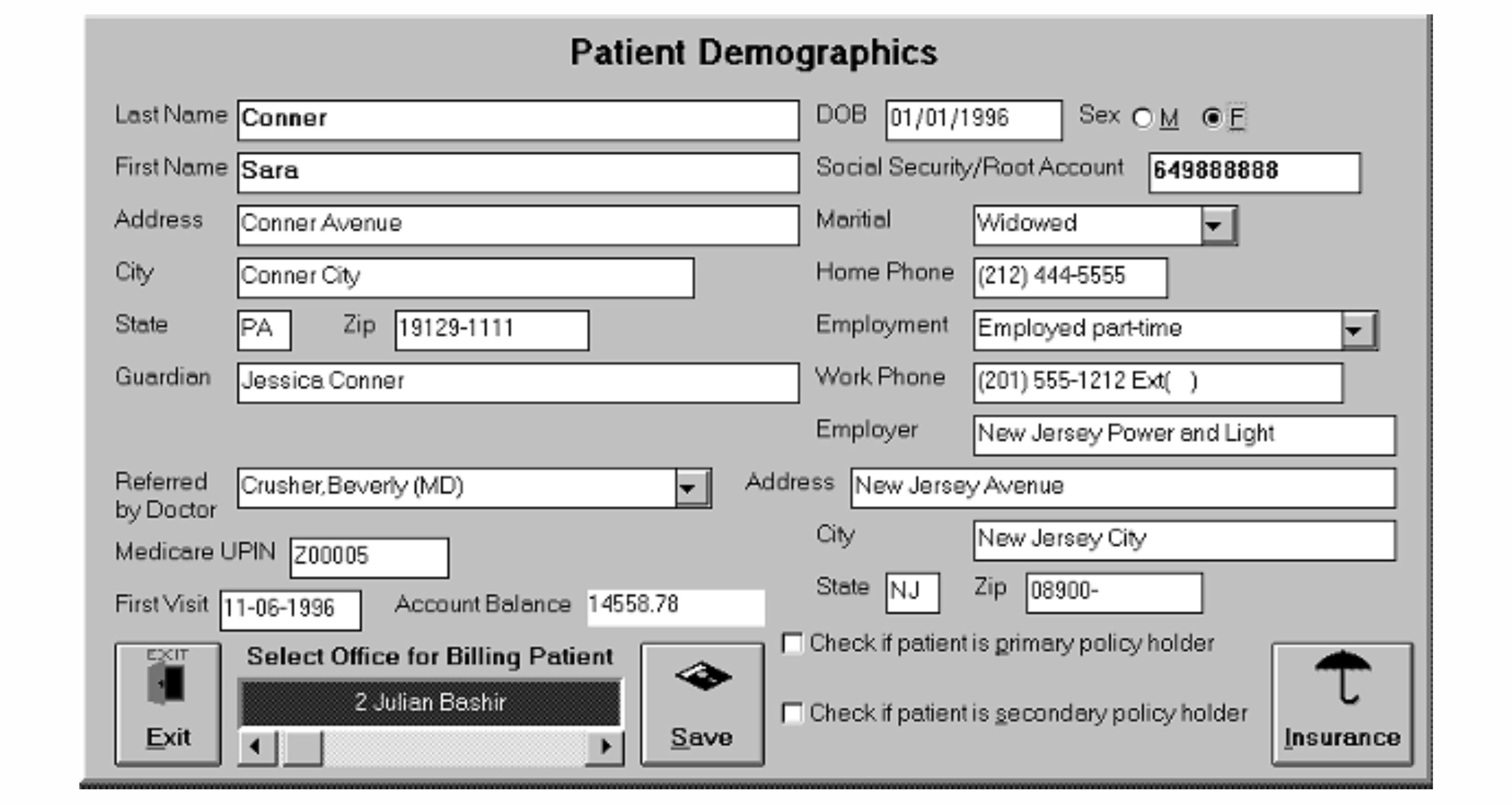
Our highly trained and qualified Data Entry Team and Quality Control Team makes sure that all data is entered exactly as provided. We understand the importance of making sure that insurance ID numbers, claims address and all demographic and insurance information is entered correctly and directly impacts claim payment.

MEDICAL CODING
Our Coders have the added knowledge of working on multi specialty practices, matching CPT codes to diagnosis codes so that the claims get paid.

CHARGE ENTRY
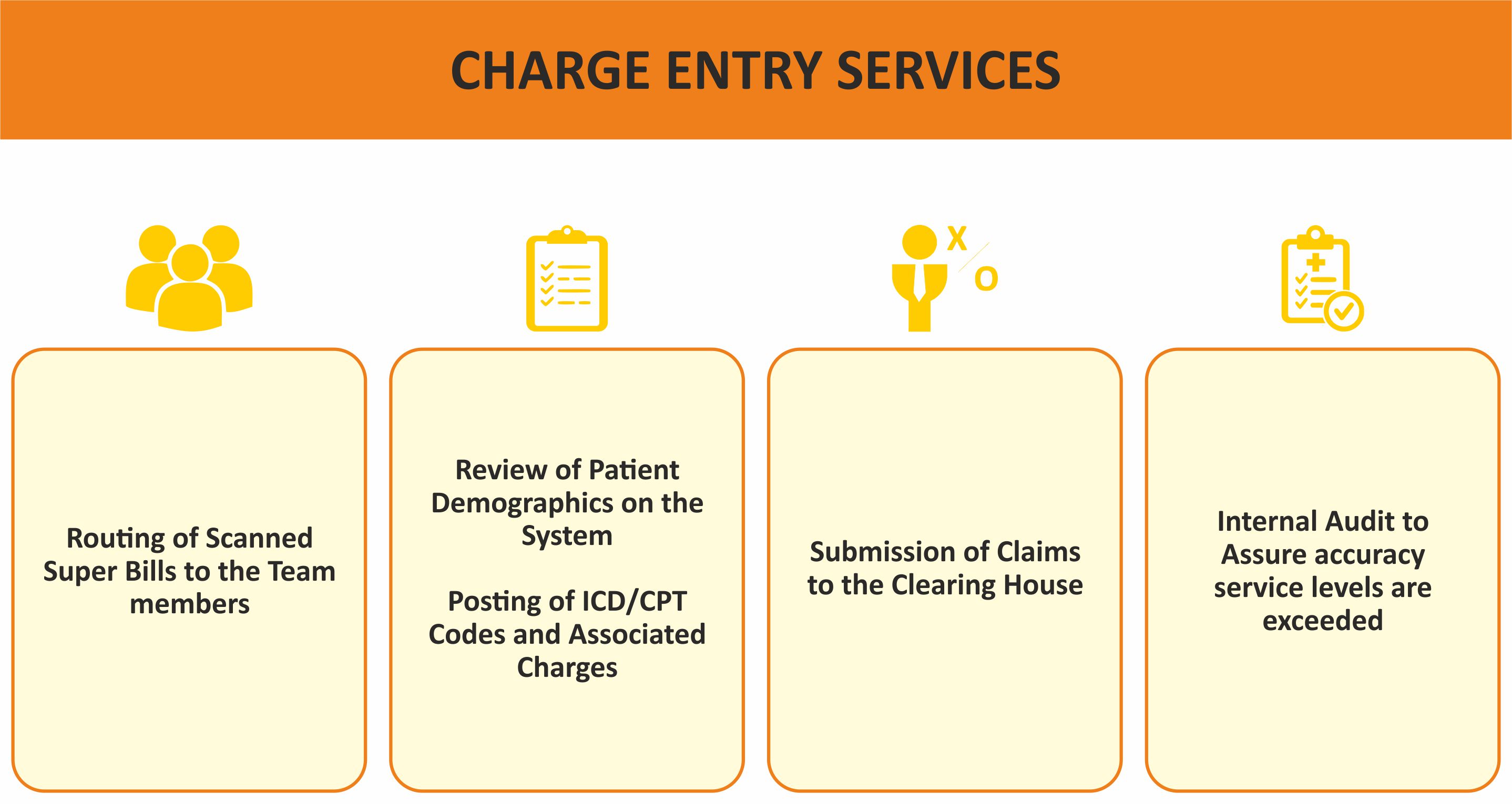
Proven Charge Entry service, we handle one of your most time-consuming and costliest priorities.We take your documented services, match them to registration data and turn it into billable fees. All with near-flawless results.

PAYMENT POSTING
We have experienced and well trained billing professionals knowledgeable of different kind of EOB’s (Explanation Of Benefits) across ALL PAYERS posting MANUAL and ELECTRONIC PAYMENTS. Payments received from Patient’s and Insurance Companies are posted to the patient accounts in the client’s medical billing system. The posted payments are balanced against the bank deposit slips to ensure payments received are reconciled on a day to day basis.

DENIAL MANAGEMENT
We turn denials into Dollars. A recent study showed more than 60% denials are recoverable. Our experienced and proactive denial management team carefully analyze your remittance advice to identify the root causes of denials, zero pays, claim reversals and meticulously work on them until the claim is closed out. Our correspondence and appeals process ensures recovery of revenue considered lost.

MINDGENIX
Mindgenix is a leading Medical Billing Company. Our medical billing services are tailored to your practice’s specific needs and we work with you and your staff as closely as an in-house biller.

DETAILED ANALYTICS
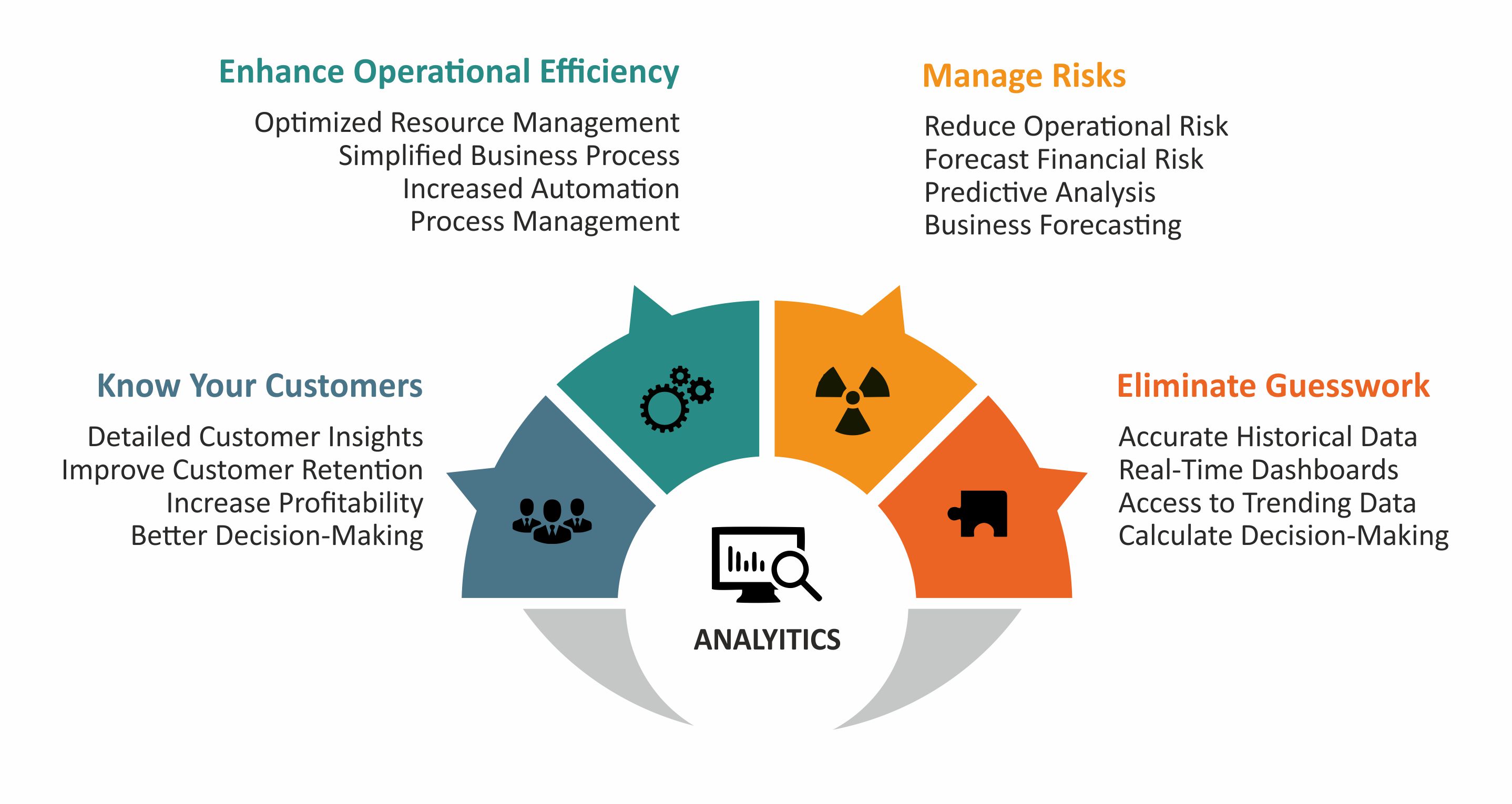
Dedicated client based dashboards and analytics to ensure the client knows what is sent and what is received along with denial management and patient collections.
NEED TO OUTSOURCE YOUR MEDICAL BILLING?
Contact us now and receive the best solutions to your requirements